

The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine (2021)
Chapter: 8 major findings and research questions, 8 major findings and research questions, introduction.
The COVID-19 pandemic, which began in late 2019, created unprecedented global disruption and infused a significant level of uncertainty into the lives of individuals, both personally and professionally, around the world throughout 2020. The significant effect on vulnerable populations, such as essential workers and the elderly, is well documented, as is the devastating effect the COVID-19 pandemic had on the economy, particularly brick-and-mortar retail and hospitality and food services. Concurrently, the deaths of unarmed Black people at the hands of law enforcement officers created a heightened awareness of the persistence of structural injustices in U.S. society.
Against the backdrop of this public health crisis, economic upheaval, and amplified social consciousness, an ad hoc committee was appointed to review the potential effects of the COVID-19 pandemic on women in academic science, technology, engineering, mathematics, and medicine (STEMM) during 2020. The committee’s work built on the National Academies of Sciences, Engineering, and Medicine report Promising Practices for Addressing the Underrepresentation of Women in Science, Engineering, and Medicine: Opening Doors (the Promising Practices report), which presents evidence-based recommendations to address the well-established structural barriers that impede the advancement of women in STEMM. However, the committee recognized that none of the actions identified in the Promising Practices report were conceived within the context of a pandemic, an economic downturn, or the emergence of national protests against structural racism. The representation and vitality of academic women in STEMM had already warranted national attention prior to these events, and the COVID-19
pandemic appeared to represent an additional risk to the fragile progress that women had made in some STEMM disciplines. Furthermore, the future will almost certainly hold additional, unforeseen disruptions, which underscores the importance of the committee’s work.
In times of stress, there is a risk that the divide will deepen between those who already have advantages and those who do not. In academia, senior and tenured academics are more likely to have an established reputation, a stable salary commitment, and power within the academic system. They are more likely, before the COVID-19 pandemic began, to have established professional networks, generated data that can be used to write papers, and achieved financial and job security. While those who have these advantages may benefit from a level of stability relative to others during stressful times, those who were previously systemically disadvantaged are more likely to experience additional strain and instability.
As this report has documented, during 2020 the COVID-19 pandemic had overall negative effects on women in academic STEMM in areas such productivity, boundary setting and boundary control, networking and community building, burnout rates, and mental well-being. The excessive expectations of caregiving that often fall on the shoulders of women cut across career timeline and rank (e.g., graduate student, postdoctoral scholar, non-tenure-track and other contingent faculty, tenure-track faculty), institution type, and scientific discipline. Although there have been opportunities for innovation and some potential shifts in expectations, increased caregiving demands associated with the COVID-19 pandemic in 2020, such as remote working, school closures, and childcare and eldercare, had disproportionately negative outcomes for women.
The effects of the COVID-19 pandemic on women in STEMM during 2020 are understood better through an intentionally intersectional lens. Productivity, career, boundary setting, mental well-being, and health are all influenced by the ways in which social identities are defined and cultivated within social and power structures. Race and ethnicity, sexual orientation, gender identity, academic career stage, appointment type, institution type, age, and disability status, among many other factors, can amplify or diminish the effects of the COVID-19 pandemic for a given person. For example, non-cisgender women may be forced to return to home environments where their gender identity is not accepted, increasing their stress and isolation, and decreasing their well-being. Women of Color had a higher likelihood of facing a COVID-19–related death in their family compared with their white, non-Hispanic colleagues. The full extent of the effects of the COVID-19 pandemic for women of various social identities was not fully understood at the end of 2020.
Considering the relative paucity of women in many STEMM fields prior to the COVID-19 pandemic, women are more likely to experience academic isolation, including limited access to mentors, sponsors, and role models that share gender, racial, or ethnic identities. Combining this reality with the physical isolation stipulated by public health responses to the COVID-19 pandemic,
women in STEMM were subject to increasing isolation within their fields, networks, and communities. Explicit attention to the early indicators of how the COVID-19 pandemic affected women in academic STEMM careers during 2020, as well as attention to crisis responses throughout history, may provide opportunities to mitigate some of the long-term effects and potentially develop a more resilient and equitable academic STEMM system.
MAJOR FINDINGS
Given the ongoing nature of the COVID-19 pandemic, it was not possible to fully understand the entirety of the short- or long-term implications of this global disruption on the careers of women in academic STEMM. Having gathered preliminary data and evidence available in 2020, the committee found that significant changes to women’s work-life boundaries and divisions of labor, careers, productivity, advancement, mentoring and networking relationships, and mental health and well-being have been observed. The following findings represent those aspects that the committee agreed have been substantiated by the preliminary data, evidence, and information gathered by the end of 2020. They are presented either as Established Research and Experiences from Previous Events or Impacts of the COVID-19 Pandemic during 2020 that parallel the topics as presented in the report.
Established Research and Experiences from Previous Events
___________________
1 This finding is primarily based on research on cisgender women and men.
Impacts of the COVID-19 Pandemic during 2020
Research questions.
While this report compiled much of the research, data, and evidence available in 2020 on the effects of the COVID-19 pandemic, future research is still needed to understand all the potential effects, especially any long-term implications. The research questions represent areas the committee identified for future research, rather than specific recommendations. They are presented in six categories that parallel the chapters of the report: Cross-Cutting Themes; Academic Productivity and Institutional Responses; Work-Life Boundaries and Gendered Divisions of Labor; Collaboration, Networking, and Professional Societies; Academic Leadership and Decision-Making; and Mental Health and Well-being. The committee hopes the report will be used as a basis for continued understanding of the impact of the COVID-19 pandemic in its entirety and as a reference for mitigating impacts of future disruptions that affect women in academic STEMM. The committee also hopes that these research questions may enable academic STEMM to emerge from the pandemic era a stronger, more equitable place for women. Therefore, the committee identifies two types of research questions in each category; listed first are those questions aimed at understanding the impacts of the disruptions from the COVID-19 pandemic, followed by those questions exploring the opportunities to help support the full participation of women in the future.
Cross-Cutting Themes
- What are the short- and long-term effects of the COVID-19 pandemic on the career trajectories, job stability, and leadership roles of women, particularly of Black women and other Women of Color? How do these effects vary across institutional characteristics, 2 discipline, and career stage?
2 Institutional characteristics include different institutional types (e.g., research university, liberal arts college, community college), locales (e.g., urban, rural), missions (e.g., Historically Black Colleges and Universities, Hispanic-Serving Institutions, Asian American/Native American/Pacific Islander-Serving Institutions, Tribal Colleges and Universities), and levels of resources.
- How did the confluence of structural racism, economic hardships, and environmental disruptions affect Women of Color during the COVID-19 pandemic? Specifically, how did the murder of George Floyd, Breonna Taylor, and other Black citizens impact Black women academics’ safety, ability to be productive, and mental health?
- How has the inclusion of women in leadership and other roles in the academy influenced the ability of institutions to respond to the confluence of major social crises during the COVID-19 pandemic?
- How can institutions build on the involvement women had across STEMM disciplines during the COVID-19 pandemic to increase the participation of women in STEMM and/or elevate and support women in their current STEMM-related positions?
- How can institutions adapt, leverage, and learn from approaches developed during 2020 to attend to challenges experienced by Women of Color in STEMM in the future?
Academic Productivity and Institutional Responses
- How did the institutional responses (e.g., policies, practices) that were outlined in the Major Findings impact women faculty across institutional characteristics and disciplines?
- What are the short- and long-term effects of faculty evaluation practices and extension policies implemented during the COVID-19 pandemic on the productivity and career trajectories of members of the academic STEMM workforce by gender?
- What adaptations did women use during the transition to online and hybrid teaching modes? How did these techniques and adaptations vary as a function of career stage and institutional characteristics?
- What are examples of institutional changes implemented in response to the COVID-19 pandemic that have the potential to reduce systemic barriers to participation and advancement that have historically been faced by academic women in STEMM, specifically Women of Color and other marginalized women in STEMM? How might positive institutional responses be leveraged to create a more resilient and responsive higher education ecosystem?
- How can or should funding arrangements be altered (e.g., changes in funding for research and/or mentorship programs) to support new ways of interaction for women in STEMM during times of disruption, such as the COVID-19 pandemic?
Work-Life Boundaries and Gendered Divisions of Labor
- How do different social identities (e.g., racial; socioeconomic status; culturally, ethnically, sexually, or gender diverse; immigration status; parents of young children and other caregivers; women without partners) influence the management of work-nonwork boundaries? How did this change during the COVID-19 pandemic?
- How have COVID-19 pandemic-related disruptions affected progress toward reducing the gender gap in academic STEMM labor-force participation? How does this differ for Women of Color or women with caregiving responsibilities?
- How can institutions account for the unique challenges of women faculty with parenthood and caregiving responsibilities when developing effective and equitable policies, practices, or programs?
- How might insights gained about work-life boundaries during the COVID-19 pandemic inform how institutions develop and implement supportive resources (e.g., reductions in workload, on-site childcare, flexible working options)?
Collaboration, Networking, and Professional Societies
- What were the short- and long-term effects of the COVID-19 pandemic-prompted switch from in-person conferences to virtual conferences on conference culture and climate, especially for women in STEMM?
- How will the increase in virtual conferences specifically affect women’s advancement and career trajectories? How will it affect women’s collaborations?
- How has the shift away from attending conferences and in-person networking changed longer-term mentoring and sponsoring relationships, particularly in terms of gender dynamics?
- How can institutions maximize the benefits of digitization and the increased use of technology observed during the COVID-19 pandemic to continue supporting women, especially marginalized women, by increasing accessibility, collaborations, mentorship, and learning?
- How can organizations that support, host, or facilitate online and virtual conferences and networking events (1) ensure open and fair access to participants who face different funding and time constraints; (2) foster virtual connections among peers, mentors, and sponsors; and (3) maintain an inclusive environment to scientists of all backgrounds?
- What policies, practices, or programs can be developed to help women in STEMM maintain a sense of support, structure, and stability during and after periods of disruption?
Academic Leadership and Decision-Making
- What specific interventions did colleges and universities initiate or prioritize to ensure that women were included in decision-making processes during responses to the COVID-19 pandemic?
- How effective were colleges and universities that prioritized equity-minded leadership, shared leadership, and crisis leadership styles at mitigating emerging and potential negative effects of the COVID-19 pandemic on women in their communities?
- What specific aspects of different leadership models translated to more effective strategies to advance women in STEMM, particularly during the COVID-19 pandemic?
- How can examples of intentional inclusion of women in decision-making processes during the COVID-19 pandemic be leveraged to develop the engagement of women as leaders at all levels of academic institutions?
- What are potential “top-down” structural changes in academia that can be implemented to mitigate the adverse effects of the COVID-19 pandemic or other disruptions?
- How can academic leadership, at all levels, more effectively support the mental health needs of women in STEMM?
Mental Health and Well-being
- What is the impact of the COVID-19 pandemic and institutional responses on the mental health and well-being of members of the academic STEMM workforce as a function of gender, race, and career stage?
- How are tools and diagnostic tests to measure aspects of wellbeing, including burnout and insomnia, used in academic settings? How does this change during times of increased stress, such as the COVID-19 pandemic?
- How might insights gained about mental health during the COVID-19 pandemic be used to inform preparedness for future disruptions?
- How can programs that focus on changes in biomarkers of stress and mood dysregulation, such as levels of sleep, activity, and texting patterns, be developed and implemented to better engage women in addressing their mental health?
- What are effective interventions to address the health of women academics in STEMM that specifically account for the effects of stress on women? What are effective interventions to mitigate the excessive levels of stress for Women of Color?
This page intentionally left blank.
The spring of 2020 marked a change in how almost everyone conducted their personal and professional lives, both within science, technology, engineering, mathematics, and medicine (STEMM) and beyond. The COVID-19 pandemic disrupted global scientific conferences and individual laboratories and required people to find space in their homes from which to work. It blurred the boundaries between work and non-work, infusing ambiguity into everyday activities. While adaptations that allowed people to connect became more common, the evidence available at the end of 2020 suggests that the disruptions caused by the COVID-19 pandemic endangered the engagement, experience, and retention of women in academic STEMM, and may roll back some of the achievement gains made by women in the academy to date.
The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine identifies, names, and documents how the COVID-19 pandemic disrupted the careers of women in academic STEMM during the initial 9-month period since March 2020 and considers how these disruptions - both positive and negative - might shape future progress for women. This publication builds on the 2020 report Promising Practices for Addressing the Underrepresentation of Women in Science, Engineering, and Medicine to develop a comprehensive understanding of the nuanced ways these disruptions have manifested. The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine will inform the academic community as it emerges from the pandemic to mitigate any long-term negative consequences for the continued advancement of women in the academic STEMM workforce and build on the adaptations and opportunities that have emerged.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
Greater Good Science Center • Magazine • In Action • In Education
11 Questions to Ask About COVID-19 Research
Debates have raged on social media, around dinner tables, on TV, and in Congress about the science of COVID-19. Is it really worse than the flu? How necessary are lockdowns? Do masks work to prevent infection? What kinds of masks work best? Is the new vaccine safe?
You might see friends, relatives, and coworkers offer competing answers, often brandishing studies or citing individual doctors and scientists to support their positions. With so much disagreement—and with such high stakes—how can we use science to make the best decisions?
Here at Greater Good , we cover research into social and emotional well-being, and we try to help people apply findings to their personal and professional lives. We are well aware that our business is a tricky one.

Summarizing scientific studies and distilling the key insights that people can apply to their lives isn’t just difficult for the obvious reasons, like understanding and then explaining formal science terms or rigorous empirical and analytic methods to non-specialists. It’s also the case that context gets lost when we translate findings into stories, tips, and tools, especially when we push it all through the nuance-squashing machine of the Internet. Many people rarely read past the headlines, which intrinsically aim to be relatable and provoke interest in as many people as possible. Because our articles can never be as comprehensive as the original studies, they almost always omit some crucial caveats, such as limitations acknowledged by the researchers. To get those, you need access to the studies themselves.
And it’s very common for findings and scientists to seem to contradict each other. For example, there were many contradictory findings and recommendations about the use of masks, especially at the beginning of the pandemic—though as we’ll discuss, it’s important to understand that a scientific consensus did emerge.
Given the complexities and ambiguities of the scientific endeavor, is it possible for a non-scientist to strike a balance between wholesale dismissal and uncritical belief? Are there red flags to look for when you read about a study on a site like Greater Good or hear about one on a Fox News program? If you do read an original source study, how should you, as a non-scientist, gauge its credibility?
Here are 11 questions you might ask when you read about the latest scientific findings about the pandemic, based on our own work here at Greater Good.
1. Did the study appear in a peer-reviewed journal?
In peer review, submitted articles are sent to other experts for detailed critical input that often must be addressed in a revision prior to being accepted and published. This remains one of the best ways we have for ascertaining the rigor of the study and rationale for its conclusions. Many scientists describe peer review as a truly humbling crucible. If a study didn’t go through this process, for whatever reason, it should be taken with a much bigger grain of salt.
“When thinking about the coronavirus studies, it is important to note that things were happening so fast that in the beginning people were releasing non-peer reviewed, observational studies,” says Dr. Leif Hass, a family medicine doctor and hospitalist at Sutter Health’s Alta Bates Summit Medical Center in Oakland, California. “This is what we typically do as hypothesis-generating but given the crisis, we started acting on them.”
In a confusing, time-pressed, fluid situation like the one COVID-19 presented, people without medical training have often been forced to simply defer to expertise in making individual and collective decisions, turning to culturally vetted institutions like the Centers for Disease Control (CDC). Is that wise? Read on.
2. Who conducted the study, and where did it appear?
“I try to listen to the opinion of people who are deep in the field being addressed and assess their response to the study at hand,” says Hass. “With the MRNA coronavirus vaccines, I heard Paul Offit from UPenn at a UCSF Grand Rounds talk about it. He literally wrote the book on vaccines. He reviewed what we know and gave the vaccine a big thumbs up. I was sold.”
From a scientific perspective, individual expertise and accomplishment matters—but so does institutional affiliation.
Why? Because institutions provide a framework for individual accountability as well as safety guidelines. At UC Berkeley, for example , research involving human subjects during COVID-19 must submit a Human Subjects Proposal Supplement Form , and follow a standard protocol and rigorous guidelines . Is this process perfect? No. It’s run by humans and humans are imperfect. However, the conclusions are far more reliable than opinions offered by someone’s favorite YouTuber .
Recommendations coming from institutions like the CDC should not be accepted uncritically. At the same time, however, all of us—including individuals sporting a “Ph.D.” or “M.D.” after their names—must be humble in the face of them. The CDC represents a formidable concentration of scientific talent and knowledge that dwarfs the perspective of any one individual. In a crisis like COVID-19, we need to defer to that expertise, at least conditionally.
“If we look at social media, things could look frightening,” says Hass. When hundreds of millions of people are vaccinated, millions of them will be afflicted anyway, in the course of life, by conditions like strokes, anaphylaxis, and Bell’s palsy. “We have to have faith that people collecting the data will let us know if we are seeing those things above the baseline rate.”
3. Who was studied, and where?
Animal experiments tell scientists a lot, but their applicability to our daily human lives will be limited. Similarly, if researchers only studied men, the conclusions might not be relevant to women, and vice versa.
Many psychology studies rely on WEIRD (Western, educated, industrialized, rich and democratic) participants, mainly college students, which creates an in-built bias in the discipline’s conclusions. Historically, biomedical studies also bias toward gathering measures from white male study participants, which again, limits generalizability of findings. Does that mean you should dismiss Western science? Of course not. It’s just the equivalent of a “Caution,” “Yield,” or “Roadwork Ahead” sign on the road to understanding.
This applies to the coronavirus vaccines now being distributed and administered around the world. The vaccines will have side effects; all medicines do. Those side effects will be worse for some people than others, depending on their genetic inheritance, medical status, age, upbringing, current living conditions, and other factors.
For Hass, it amounts to this question: Will those side effects be worse, on balance, than COVID-19, for most people?
“When I hear that four in 100,000 [of people in the vaccine trials] had Bell’s palsy, I know that it would have been a heck of a lot worse if 100,000 people had COVID. Three hundred people would have died and many others been stuck with chronic health problems.”
4. How big was the sample?
In general, the more participants in a study, the more valid its results. That said, a large sample is sometimes impossible or even undesirable for certain kinds of studies. During COVID-19, limited time has constrained the sample sizes.
However, that acknowledged, it’s still the case that some studies have been much larger than others—and the sample sizes of the vaccine trials can still provide us with enough information to make informed decisions. Doctors and nurses on the front lines of COVID-19—who are now the very first people being injected with the vaccine—think in terms of “biological plausibility,” as Hass says.
Did the admittedly rushed FDA approval of the Pfizer-BioNTech vaccine make sense, given what we already know? Tens of thousands of doctors who have been grappling with COVID-19 are voting with their arms, in effect volunteering to be a sample for their patients. If they didn’t think the vaccine was safe, you can bet they’d resist it. When the vaccine becomes available to ordinary people, we’ll know a lot more about its effects than we do today, thanks to health care providers paving the way.
5. Did the researchers control for key differences, and do those differences apply to you?
Diversity or gender balance aren’t necessarily virtues in experimental research, though ideally a study sample is as representative of the overall population as possible. However, many studies use intentionally homogenous groups, because this allows the researchers to limit the number of different factors that might affect the result.
While good researchers try to compare apples to apples, and control for as many differences as possible in their analyses, running a study always involves trade-offs between what can be accomplished as a function of study design, and how generalizable the findings can be.

The Science of Happiness
What does it take to live a happier life? Learn research-tested strategies that you can put into practice today. Hosted by award-winning psychologist Dacher Keltner. Co-produced by PRX and UC Berkeley’s Greater Good Science Center.
- Apple Podcasts
- Google Podcasts
You also need to ask if the specific population studied even applies to you. For example, when one study found that cloth masks didn’t work in “high-risk situations,” it was sometimes used as evidence against mask mandates.
However, a look beyond the headlines revealed that the study was of health care workers treating COVID-19 patients, which is a vastly more dangerous situation than, say, going to the grocery store. Doctors who must intubate patients can end up being splattered with saliva. In that circumstance, one cloth mask won’t cut it. They also need an N95, a face shield, two layers of gloves, and two layers of gown. For the rest of us in ordinary life, masks do greatly reduce community spread, if as many people as possible are wearing them.
6. Was there a control group?
One of the first things to look for in methodology is whether the population tested was randomly selected, whether there was a control group, and whether people were randomly assigned to either group without knowing which one they were in. This is especially important if a study aims to suggest that a certain experience or treatment might actually cause a specific outcome, rather than just reporting a correlation between two variables (see next point).
For example, were some people randomly assigned a specific meditation practice while others engaged in a comparable activity or exercise? If the sample is large enough, randomized trials can produce solid conclusions. But, sometimes, a study will not have a control group because it’s ethically impossible. We can’t, for example, let sick people go untreated just to see what would happen. Biomedical research often makes use of standard “treatment as usual” or placebos in control groups. They also follow careful ethical guidelines to protect patients from both maltreatment and being deprived necessary treatment. When you’re reading about studies of masks, social distancing, and treatments during the COVID-19, you can partially gauge the reliability and validity of the study by first checking if it had a control group. If it didn’t, the findings should be taken as preliminary.
7. Did the researchers establish causality, correlation, dependence, or some other kind of relationship?
We often hear “Correlation is not causation” shouted as a kind of battle cry, to try to discredit a study. But correlation—the degree to which two or more measurements seem connected—is important, and can be a step toward eventually finding causation—that is, establishing a change in one variable directly triggers a change in another. Until then, however, there is no way to ascertain the direction of a correlational relationship (does A change B, or does B change A), or to eliminate the possibility that a third, unmeasured factor is behind the pattern of both variables without further analysis.
In the end, the important thing is to accurately identify the relationship. This has been crucial in understanding steps to counter the spread of COVID-19 like shelter-in-place orders. Just showing that greater compliance with shelter-in-place mandates was associated with lower hospitalization rates is not as conclusive as showing that one community that enacted shelter-in-place mandates had lower hospitalization rates than a different community of similar size and population density that elected not to do so.
We are not the first people to face an infection without understanding the relationships between factors that would lead to more of it. During the bubonic plague, cities would order rodents killed to control infection. They were onto something: Fleas that lived on rodents were indeed responsible. But then human cases would skyrocket.
Why? Because the fleas would migrate off the rodent corpses onto humans, which would worsen infection. Rodent control only reduces bubonic plague if it’s done proactively; once the outbreak starts, killing rats can actually make it worse. Similarly, we can’t jump to conclusions during the COVID-19 pandemic when we see correlations.
8. Are journalists and politicians, or even scientists, overstating the result?
Language that suggests a fact is “proven” by one study or which promotes one solution for all people is most likely overstating the case. Sweeping generalizations of any kind often indicate a lack of humility that should be a red flag to readers. A study may very well “suggest” a certain conclusion but it rarely, if ever, “proves” it.
This is why we use a lot of cautious, hedging language in Greater Good , like “might” or “implies.” This applies to COVID-19 as well. In fact, this understanding could save your life.
When President Trump touted the advantages of hydroxychloroquine as a way to prevent and treat COVID-19, he was dramatically overstating the results of one observational study. Later studies with control groups showed that it did not work—and, in fact, it didn’t work as a preventative for President Trump and others in the White House who contracted COVID-19. Most survived that outbreak, but hydroxychloroquine was not one of the treatments that saved their lives. This example demonstrates how misleading and even harmful overstated results can be, in a global pandemic.
9. Is there any conflict of interest suggested by the funding or the researchers’ affiliations?
A 2015 study found that you could drink lots of sugary beverages without fear of getting fat, as long as you exercised. The funder? Coca Cola, which eagerly promoted the results. This doesn’t mean the results are wrong. But it does suggest you should seek a second opinion : Has anyone else studied the effects of sugary drinks on obesity? What did they find?
It’s possible to take this insight too far. Conspiracy theorists have suggested that “Big Pharma” invented COVID-19 for the purpose of selling vaccines. Thus, we should not trust their own trials showing that the vaccine is safe and effective.
But, in addition to the fact that there is no compelling investigative evidence that pharmaceutical companies created the virus, we need to bear in mind that their trials didn’t unfold in a vacuum. Clinical trials were rigorously monitored and independently reviewed by third-party entities like the World Health Organization and government organizations around the world, like the FDA in the United States.
Does that completely eliminate any risk? Absolutely not. It does mean, however, that conflicts of interest are being very closely monitored by many, many expert eyes. This greatly reduces the probability and potential corruptive influence of conflicts of interest.
10. Do the authors reference preceding findings and original sources?
The scientific method is based on iterative progress, and grounded in coordinating discoveries over time. Researchers study what others have done and use prior findings to guide their own study approaches; every study builds on generations of precedent, and every scientist expects their own discoveries to be usurped by more sophisticated future work. In the study you are reading, do the researchers adequately describe and acknowledge earlier findings, or other key contributions from other fields or disciplines that inform aspects of the research, or the way that they interpret their results?

Greater Good’s Guide to Well-Being During Coronavirus
Practices, resources, and articles for individuals, parents, and educators facing COVID-19
This was crucial for the debates that have raged around mask mandates and social distancing. We already knew quite a bit about the efficacy of both in preventing infections, informed by centuries of practical experience and research.
When COVID-19 hit American shores, researchers and doctors did not question the necessity of masks in clinical settings. Here’s what we didn’t know: What kinds of masks would work best for the general public, who should wear them, when should we wear them, were there enough masks to go around, and could we get enough people to adopt best mask practices to make a difference in the specific context of COVID-19 ?
Over time, after a period of confusion and contradictory evidence, those questions have been answered . The very few studies that have suggested masks don’t work in stopping COVID-19 have almost all failed to account for other work on preventing the disease, and had results that simply didn’t hold up. Some were even retracted .
So, when someone shares a coronavirus study with you, it’s important to check the date. The implications of studies published early in the pandemic might be more limited and less conclusive than those published later, because the later studies could lean on and learn from previously published work. Which leads us to the next question you should ask in hearing about coronavirus research…
11. Do researchers, journalists, and politicians acknowledge limitations and entertain alternative explanations?
Is the study focused on only one side of the story or one interpretation of the data? Has it failed to consider or refute alternative explanations? Do they demonstrate awareness of which questions are answered and which aren’t by their methods? Do the journalists and politicians communicating the study know and understand these limitations?
When the Annals of Internal Medicine published a Danish study last month on the efficacy of cloth masks, some suggested that it showed masks “make no difference” against COVID-19.
The study was a good one by the standards spelled out in this article. The researchers and the journal were both credible, the study was randomized and controlled, and the sample size (4,862 people) was fairly large. Even better, the scientists went out of their way to acknowledge the limits of their work: “Inconclusive results, missing data, variable adherence, patient-reported findings on home tests, no blinding, and no assessment of whether masks could decrease disease transmission from mask wearers to others.”
Unfortunately, their scientific integrity was not reflected in the ways the study was used by some journalists, politicians, and people on social media. The study did not show that masks were useless. What it did show—and what it was designed to find out—was how much protection masks offered to the wearer under the conditions at the time in Denmark. In fact, the amount of protection for the wearer was not large, but that’s not the whole picture: We don’t wear masks mainly to protect ourselves, but to protect others from infection. Public-health recommendations have stressed that everyone needs to wear a mask to slow the spread of infection.
“We get vaccinated for the greater good, not just to protect ourselves ”
As the authors write in the paper, we need to look to other research to understand the context for their narrow results. In an editorial accompanying the paper in Annals of Internal Medicine , the editors argue that the results, together with existing data in support of masks, “should motivate widespread mask wearing to protect our communities and thereby ourselves.”
Something similar can be said of the new vaccine. “We get vaccinated for the greater good, not just to protect ourselves,” says Hass. “Being vaccinated prevents other people from getting sick. We get vaccinated for the more vulnerable in our community in addition for ourselves.”
Ultimately, the approach we should take to all new studies is a curious but skeptical one. We should take it all seriously and we should take it all with a grain of salt. You can judge a study against your experience, but you need to remember that your experience creates bias. You should try to cultivate humility, doubt, and patience. You might not always succeed; when you fail, try to admit fault and forgive yourself.
Above all, we need to try to remember that science is a process, and that conclusions always raise more questions for us to answer. That doesn’t mean we never have answers; we do. As the pandemic rages and the scientific process unfolds, we as individuals need to make the best decisions we can, with the information we have.
This article was revised and updated from a piece published by Greater Good in 2015, “ 10 Questions to Ask About Scientific Studies .”
About the Authors
Jeremy Adam Smith
Uc berkeley.
Jeremy Adam Smith edits the GGSC’s online magazine, Greater Good . He is also the author or coeditor of five books, including The Daddy Shift , Are We Born Racist? , and (most recently) The Gratitude Project: How the Science of Thankfulness Can Rewire Our Brains for Resilience, Optimism, and the Greater Good . Before joining the GGSC, Jeremy was a John S. Knight Journalism Fellow at Stanford University.
Emiliana R. Simon-Thomas
Emiliana R. Simon-Thomas, Ph.D. , is the science director of the Greater Good Science Center, where she directs the GGSC’s research fellowship program and serves as a co-instructor of its Science of Happiness and Science of Happiness at Work online courses.
You May Also Enjoy

Why Is COVID-19 Killing So Many Black Americans?

Why Your Sacrifices Matter During the Pandemic

In a Pandemic, Elbow Touches Might Keep Us Going

How to Keep the Greater Good in Mind During the Coronavirus Outbreak

How Does COVID-19 Affect Trust in Government?

How to Form a Pandemic Pod

An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

SARS-CoV-2 and COVID-19: revisiting the most important research questions
Kit-san yuen, sin-yee fung, pak-hin hinson cheung, chi-ping chan, dong-yan jin.
- Author information
- Article notes
- Copyright and License information
Corresponding author.
Received 2021 Dec 2; Accepted 2021 Dec 11; Collection date 2021.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
In February 2020, we highlighted the top nine important research questions on SARS-CoV-2 and COVID-19 concerning virus transmission, asymptomatic and presymptomatic virus shedding, diagnosis, treatment, vaccine development, origin of virus and viral pathogenesis. These and related questions are revisited at the end of 2021 to shed light on the roadmap of bringing an end to the pandemic.
Keywords: SARS-CoV-2, COVID-19, Pandemic, Endemic, Vaccines, Antivirals
When only slightly more than 80,000 confirmed cases of SARS-CoV-2 infection were reported worldwide and right before COVID-19 was declared a pandemic by the WHO, we discussed the nine most important research questions on SARS-CoV-2 and COVID-19, in our commentary that was published in Cell & Bioscience at the end of February 2020 [ 1 ]. These questions are:
How was SARS-CoV-2 transmitted in Wuhan?
How transmissible and pathogenic is SARS-CoV-2 after passages in humans?
How important is asymptomatic and presymptomatic virus shedding in SARS-CoV-2 transmission?
Is fecal-oral route important in SARS-CoV-2 transmission?
How should COVID-19 be diagnosed and what diagnostic reagents should be made available?
How should COVID-19 be treated and what treatment options should be made available?
Are inactivated vaccines a viable option for SARS-CoV-2?
What were the origins of SARS-CoV-2 and COVID-19?
Why is SARS-CoV-2 less pathogenic compared to SARS-CoV?
Science has contributed substantially to the battle against COVID-19 in the past two years. Particularly, prophylactic vaccines and therapeutic drugs have been made available quickly, which have brought about and will continue to bring about a big difference in prevention and control of COVID-19. At the end of 2021, we have much better answers to all nine questions listed above and asked at the beginning of 2020. The recent efforts in our research community are also reflected in the Special Issue in Cell & Bioscience dedicated to “Frontiers in Virology and COVID-19”. As a preface to the Special Issue, we will revisit the nine research questions and other related issues. This will not only give an account of how far we have gone since early 2020, but also provide a personal perspective of what is needed to end the pandemic.
Concerning the first question about SARS-CoV-2 transmission pattern in Wuhan, results from population-level testing of antibodies against SARS-CoV-2 conducted in mid-2020 in residents of Wuhan [ 2 ] have confirmed several of our initial predictions. First, since 82.1% of infected individuals were asymptomatic as confirmed by the study [ 2 ], the numbers of undiagnosed infected people and asymptomatic carriers would be much higher than the original estimates. Second, the rise in the number of confirmed cases in Wuhan after lockdown was plausibly ascribed to multiple reasons including high basal number of infected people before the lockdown and high attack rate within families. Third, the decision to lock down Wuhan and nearby cities was extraordinary, but lifesaving. It was based on key scientific evidence obtained in January 2020 from Shenzhen [ 3 ] and the visionary prediction that the scale of the outbreak was already much bigger than what was recognized. Reconstruction of the transmission chains in 1178 patients with COVID-19 diagnosed in early 2020 in Hunan is most revealing about the role of superspreading in the transmissions of SARS-CoV-2 [ 4 ]. Hunan is a Chinese province next to Hubei, to which the city of Wuhan belongs. Importantly, 80% of the secondary infections were caused by only 15% of the infected individuals, whereas most of the remaining 85% did not transmit the virus to anyone else. About 80% of the droplets and aerosol particles that contain SARS-CoV-2 were emitted by 20% of infected people. More droplets and aerosols are generated by people who are older, obese or immunocompromised. Subjects who have higher lung capacities, speak louder, are physically more active or are singing also emit more virus than their counterparts. From another perspective, about 90% of the SARS-CoV-2 virus circulating in the communities at any given time was carried by only 2% of infected people, who have the potential to become superspreaders. At least 50% of the remaining individuals tested positive for SARS-CoV-2 RNA are non-contagious. Consistently, a small subset of people account for the biggest share of transmissions. It is particularly noteworthy that superspreading commonly occurs unexpectedly in people who have mild or no symptoms. The pandemic is fueled by active transmission in young, healthy and mobile groups of people. Based on the understanding that about 10% of the locations account for 80% of the transmissions, control measures that target transmission hotspots such as restaurants, cafes, gyms, karaoke spots and party rooms are most effective in curtailing the pandemic, when compared to a complete lockdown. Obviously, these hotspots vary in different places. For example, superspreading events have also occurred in different settings such as construction sites, labor-intensive firms, food production facilities, schools, prisons, religious gatherings, multilevel marketing activities, dancing classes and dormitories, where many people are crowded into confined and poorly ventilated spaces. In this regard, the Japanese approach of “avoiding the three Cs (closed spaces, crowded places and close-contact settings)” has also been successful in preventing explosive outbreaks. Hence, it will be much more effective if mitigations are specifically designed and executed to target superspreading rather than to achieve and maintain a SARS-CoV-2-free status. For example, identification and quarantine of people with high viral loads are much more cost-effective and efficient in the prevention of superspreading and explosive outbreaks, if compared to blocking all visitors from outside of the country or quarantining them blindly for 28 days.
We have most answers to the second question concerning transmissibility and pathogenicity of SARS-CoV-2 after passages in humans. Highly transmissible variants of SARS-CoV-2 such as D614G and Alpha variants have quickly replaced the original Wuhan strain worldwide, but they gave way to the highly fit and even more transmissible Delta variant, which accounts for 99% of sequenced COVID-19 cases globally at present. It remains to be seen whether the Omicron variant newly identified from South Africa and carrying more than 50 point mutations in the genome, among which more than 30 are in the spike region, might outcompete Delta to become the next predominant strain in the near future. Noteworthily, the pathogenicity of most if not all highly transmissible strains does not increase. More and more people have developed immunity against SARS-CoV-2 through vaccination and/or natural infection. Although breakthrough infections can still occur when neutralizing antibodies wane or are intrinsically insufficient due to different reasons, in most cases severity of disease decreases substantially. Thus, COVID-19 will be more and more like common cold caused by community-acquired human coronaviruses. In support of this notion, an analysis of 569,742 cases of COVID-19 collected from multiple sites in US indicated a death rate of 0.1% among vaccinated people infected with Delta variant of COVID-19 [ 5 ], which is much lower than those of 1.3% or 1.6% among unvaccinated people and comparable to that of seasonal influenza. Thus, even if the pathogenicity of Delta variant remains unchanged compared to that of the original strain, it will cause less harm where rates of vaccination and/or previous natural infection are high. This is very similar to the 1918 pandemic strain of influenza. Although it is highly pathogenic, the 1918 pandemic virus will not cause another pandemic now since existing immunity against it is strong and widespread among healthy people of different age groups.
The importance of asymptomatic and presymptomatic virus shedding in SARS-CoV-2 transmission, which was the third question asked in early 2020, has now been fully established. Asymptomatic and presymptomatic virus shedding poses a great challenge to infection control [ 3 ]. A small subset of asymptomatic and presymptomatic people infected with SARS-CoV-2 shed a large amount of virus and are potential superspreaders. It is also noteworthy that SARS-CoV-2 establishes a persistent infection and undergoes rapid evolution in severely immunocompromised people, giving rise to mutations that foreshadow the circulating variants [ 6 ]. Indeed, many variants of concern and variants of interest, including the newly identified Omicron variant, are thought to be arisen from immunocompromised subjects. Thus, immunocompromised individuals persistently infected with SARS-CoV-2 should be closely monitored. Uninfected but immunocompromised people should be given the priority to receive booster vaccination as many times as required. Persistent infection in some immunocompromised people might account for a small subset of cases suffering from long COVID-19. The term has no strict definition and usually refers to conditions when new and ongoing symptoms of COVID-19 are seen four or more weeks after the first onset. Some people either having long COVID-19 or being asymptomatic could be tested positive for SARS-CoV-2 RNA long after the first infection. However, if the viral titer is low, the viral RNA detected could be derived from viral gene fragments or non-functional pieces. These people with low viral titers are therefore considered non-contagious or minimally contagious.
Concerning the fourth question, we have a much better understanding of the transmission routes of SARS-CoV-2 now compared to two years ago. CDC categorizes modes of SARS-CoV-2 transmission as inhalation of droplets and aerosol particles that contain virus; deposition of droplets and aerosols on exposed mucous membranes in the nose, mouth and eyes; and touching the mucous membranes with soiled hands contaminated with virus either directly via droplets and aerosols or indirectly by touching surfaces. The definitions of droplets of more than 100 μm in diameter and aerosols of less than 100 μm have been updated. Whereas droplets are liquid particles that settle out of the air within seconds and minutes, aerosols are stable suspension of solid and/or liquid particles dried from fine droplets and capable of staying from minutes to hours. Airborne transmission has been verified as one major route for the spread of SARS-CoV-2. Particularly, as mentioned above, enclosed spaces with inadequate ventilation or air conditioning are high-risk spots for superspreading. In contrast, transmission of SARS-CoV-2 via contaminated surfaces, including packaging materials, frozen or chilled seafoods and meats, is not known to contribute substantially to new infections. In this regard, the hypothesis that several outbreaks in China and even the original one connected to the Huanan Seafood Wholesale Market in Wuhan were caused by imported foods or materials contaminated with SARS-CoV-2, has to be supported by more direct and concrete evidence. Gastrointestinal symptoms such as diarrhea, vomiting and abdominal pain are not uncommon but can be seen in up to 20% of all patients. Prolonged shedding of SARS-CoV-2 from gastrointestinal tract for as long as a month has been observed in a subset of adult and pediatric patients who are either symptomatic or asymptomatic. Interestingly, gastrointestinal involvement appears to alleviate the severity and reduce the mortality of disease to some extent. Although detection of viral RNA in sewage has been used successfully to trace infected individuals, prolonged virus shedding in the feces of convalescent and other lowly contagious patients raises a concern about its role in the prevention of superspreading. Circumstantial evidence in support of fecal-oral transmission of SARS-CoV-2 has been found in different settings such as transmission chains in high-rise buildings. However, this does not change the three main routes of transmission summarized above or the prevention methods including physical distancing, use of surgical masks, adequate ventilation, good hand hygiene and avoidance of 3Cs. SARS-CoV-2 in the feces might be transmitted via inhalation, disposition on the mucous membrane or touching the mucous membrane with contaminated hands. For the first two modes of transmission, virus in the feces has to be aerosolized.
As far as question five is concerned, all desired diagnostic reagents for SARS-CoV-2 infection have now been made available. Whereas quantitative RT-PCR analysis of SARS-CoV-2 RNA remains the gold standard in diagnosing SARS-CoV-2 infection, antigen and antibody tests also play critical roles in rapid screening, contact tracing, early detection of superspreading, assessment of immune protection and formulation of vaccination strategies. There is a need to sequence more SARS-CoV-2-positive samples for better identification and tracking of variants of concern and variants of interest, and for reconstitution of transmission chains. At present, this is particularly important in the monitoring of Omicron variant in Africa and elsewhere. Schemes and parameters for risk stratification are also required. For example, the lower the viral RNA titer, the lower the risk of transmission or superspreading. Based on this generally accepted concept, people with a very high Ct value in viral RNA detection (e.g. >30) and detectable neutralizing antibodies (e.g. measured by the surrogate test for antibodies directing against receptor-binding domain) might be exempted for quarantine.
For the sixth question concerning treatment options, two anti-SARS-CoV-2 agents have just been shown effective in clinical trials. In addition to remdesivir, corticosteroids and neutralizing antibodies that are already in clinical use, they promise to provide new treatment options to patients with COVID-19, particularly those who have higher risks of progressing to severe disease. The first oral anti-SARS-CoV-2 drug known as molnupiravir developed by Merck is a nucleoside analog that targets RNA-dependent RNA polymerase of SARS-CoV-2 to boost RNA mutagenesis [ 7 ]. It is just approved in November 2021 by UK’s regulatory agency for the treatment of mild-to-moderate COVID-19 in adults with a positive SARS-CoV-2 diagnostic test and who have at least one risk factor for developing severe disease. Prior to this, remdesivir and two monoclonal antibodies were first approved for clinical use in October 2020. The second oral anti-SARS-CoV-2 drug named poxlovid developed by Pfizer is a protease inhibitor that targets the main protease of SARS-CoV-2. It binds covalently to the catalytic cysteine residue of main protease. It is also known that the combination of poxlovid with ritonavir decelerates metabolism of poxlovid. Pfizer is currently seeking approval for emergency use of poxlovid from FDA. Molnupiravir and poxlovid are new weapons in the battle against COVID-19. They will be on the market in the coming weeks. However, they have to be used as early as practically possible after infection to have optimal beneficial effect. Since molnupiravir can evade or overcome the action of the proofreading enzyme of SARS-CoV-2, it might be more difficult for the virus to develop resistance [ 8 ]. However, it remains to be seen how quickly or how efficiently SARS-CoV-2 might develop resistance against molnupiravir or poxlovid after their widespread use.
Rapid development of effective vaccines against SARS-CoV-2 is heralded as one major scientific achievement in our battle to conquer COVID-19. We asked in our original question seven whether inactivated vaccines are a viable option for SARS-CoV-2. Indeed, they are a viable option, but mRNA vaccines, adenoviral vectored vaccines and subunit vaccines are not only feasible, but also superior as far as efficacy and duration of protection are concerned. Both mRNA vaccines and adenoviral vectored vaccines are the first-in-class approved for human use, so they truly represent major breakthroughs in molecular approaches to vaccine development. In contrast, although the inactivated vaccines can also elicit neutralizing antibodies, the titers of these antibodies are much lower compared to those in recipients of mRNA vaccines and in people recovered from moderate to severe COVID-19. As a result, the neutralizing antibodies wane to almost zero in almost all vaccinees within three months. Thus, similar to asymptomatic carriers with low viral titers, one or more booster vaccinations are required for recipients of inactivated vaccines. It remains to be determined whether additional booster injections have to be given on a regular basis. Plausibly, there should be much room for improvement in further refinement of the inactivated vaccines. In particular, the efficacy and duration of protection might be increased by elevating the dose of antigen, optimizing the use of adjuvants, optimizing the intervals between the first and second or between the second and third injections, as well as mixing and matching with other types of vaccines including mRNA, adenoviral vectored and subunit vaccines. The whole process through which an mRNA vaccine elicits humoral and cellular immunity resembles what happens when spike protein is expressed from the subgenomic RNA of SARS-CoV-2 during natural infection. In addition, the use of a very high dose of mRNA ensures that an overwhelming amount of spike protein is expressed and recognized by the host. Although mRNA vaccines are highly effective, they cannot stimulate mucosal and sterilizing immunity required for eradication of SARS-CoV-2 from humans. Thus, in addition to the development of variant-specific mRNA vaccines, particularly those targeting Delta and Omicron variants, which are already in the pipeline, live attenuated vaccines, replication-defective vaccines and single-cycle vaccines that can elicit mucosal immunity should continue to be explored. The widespread use of mRNA vaccines also provides an opportunity for booster immunization with these mucosal vaccines that are administered intranasally. This reminds us of the past success in the combination of Salk and Sabin vaccines in the near-eradication of poliovirus. Although cell-mediated immunity might still play a role in the alleviation of severe disease, neutralizing antibodies are the generally accepted correlates of immune protection against SARS-CoV-2 infection and symptomatic COVID-19. Estimates of neutralizing antibody levels required to prevention infection or severe COVID-19 are also available [ 9 ]. The tendency of the COVID-19 pandemic to become endemic just like the four community-acquired human coronaviruses, namely 229E, OC43, HKU1 and NL63 is evident. SARS-CoV-2 will unlikely be eradicated from humans in the near future. Eradication might not be necessary if the mortality is lower than 0.1%. However, eradication remains possible as long as our next-generation vaccines are sufficiently good. Effective vaccines against SARS-CoV-2 have been available, although some are more effective than the others. Increasing the production of the most effective vaccines, increasing vaccine accessibility in resource-limited countries, and educating the general public about the effectiveness and safety profiles of vaccines are three important tasks that hold the key to putting an end to the pandemic. There are new opportunities for international leaders and the WHO to show leadership and determination. Pooling vaccine manufacturing capabilities to make the most effective vaccines is in the best interest of all people on the globe. A mechanism to determine how vaccines should be made to target predominant variants, similar to the existing one by which WHO recommends the composition of the influenza vaccines for the next annual season, should also be considered and implemented. Vaccine hesitancy has become one major threat to our effort to curtail the pandemic. Scientists have a role to play here and have to work together with all stake holders to appeal to the different groups and to relieve their key concerns. Vaccination schemes have to be designed specifically for the immunocompromised and the adolescent groups to ensure high effectiveness and safety. The benefits that outweigh the risks should be explained more explicitly, transparently, and effectively to people in high-risk groups including those who are elderly, pregnant, immunocompromised, or suffering from chronic underlying diseases.
Our original response to the eighth question regarding the origins of SARS-CoV-2 and COVID-19 is still valid. Little progress has been made in the past 2 years. Since all wild animal markets have been banned and all wild animals kept in the markets have been slaughtered in China, it is well possible that the intermediate and amplifying hosts of SARS-CoV-2, similar to civets in the case of SARS-CoV, could never be found. In support of this, no wild or farmed civets, except the ones captured in one wild animal market in Shenzhen in 2003, have been found to carry SARS-CoV. However, if a reservoir host for SARS-CoV-2 exists just as dromedary in the case of MERS-CoV, it might take a bit longer to identify it. Only time will tell what is right. Concerning the origin of COVID-19 in Wuhan, we don’t think that we have the first-hand data to make any judgement on patient zero or the role of Huanan Seafood Wholesale Market, other wild animal markets, or any other places. For Huanan Seafood Wholesale Market, it remains elusive as to whether many confirmed cases were linked to a particular type of seafood and whether any infected individual was exposed to wild animal. The existence of a human superspreader in the market should also be seriously investigated. In this regard, it is of some interest to see the recent identification of a female seafood vendor at Huanan Market as the possible patient zero whose symptom onset was on December 10, 2019 [ 10 ]. However, since most infected people in Wuhan were asymptomatic and undiagnosed [ 2 ] and new cases dated back to December 2019 or even earlier were retrospectively identified, only those who have access to the first-hand data can answer whether she would be the bona fide patient zero. It is not surprising that more patients with symptom onsets earlier than December 10 have been discovered or remain to be discovered. Without thorough reassessment and release of the full dataset, analysis on the early cases in Wuhan remains incomplete and too speculative. Due to the tremendous impact of the pandemic on world economy and public health, it is imperative that Chinese and international experts should be given full access to the key original data of all early patients.
The ninth question concerning why SARS-CoV-2 is less pathogenic remains to be addressed by new thoughts and experiments. This is a long-term goal that will keep us busy in years. In this regard, one top priority is to verify whether and why Omicron variant might be less pathogenic. In addition to the comparative analysis of different viruses of SARS-CoV-2 and SARS-CoV as suggested earlier, comparison of the different hosts might also be instructive. SARS-CoV-2 is non-pathogenic in bats. Comparing bats and humans for interferon antagonism and inflammasome activation capability of SARS-CoV-2 might reveal how bats evade immunopathogenic outcome of SARS-CoV-2 infection. This might enlighten us about what critical pathways and mechanisms should be targeted to relieve SARS-CoV-2 pathogenesis in humans. New knowledge about SARS-CoV-2 pathogenesis particularly in terms of interferon antagonism and inflammasome activation will lay the foundation for rational design and development of vaccines and antivirals against SARS-CoV-2. For example, recombinant SARS-CoV-2 lacking some particular interferon antagonists or inflammasome activators are excellent candidates of live attenuation vaccines. Indeed, NSP16-deficient SARS-CoV-2 is attenuated in vitro and in animals (our unpublished data). NSP16 is a 2’-O-methyltransferase and an interferon antagonist. Further optimization of this candidate strain might result in a live attenuated vaccine against SARS-CoV-2.
SARS-CoV-2 was initially isolated in Wuhan. China should be commended for effectively eliminating SARS-CoV-2 from the communities, keeping them SARS-CoV-2-free for almost two years, producing the highest quantities of vaccines in the world and vaccinating billions of people. These great achievements are shadowed by errors, misjudgments, incompetencies and other weaknesses, particularly seen in the initial phase of the response to the outbreak in Wuhan. Malfunctioning of the National Communicable Disease Reporting System, time lag in recognizing the high transmissibility of SARS-CoV-2 and lack of communication between different groups of healthcare professionals are just a few examples. China was not alone in making some of the mistakes, which were repeated later elsewhere. Chinese inactivated vaccines are safe and effective, particularly after three or more injections. China has provided effective vaccines to Chinese people and many others who have no access to any other SARS-CoV-2 vaccines. In this sense, Chinese inactivated vaccines are saving lives. However, as discussed above, the neutralizing antibody titers elicited by these vaccines are not sufficiently high. Booster injections are required, and alternative strategies to improve their performance and to develop next-generation vaccines should be actively explored. Another open question concerns whether the zero-tolerance policy in the control of COVID-19 is sustainable. The benefits and harms of this policy versus that of “living with SARS-CoV-2” should be carefully considered and openly debated. The tendency of SARS-CoV-2 to become endemic and the low mortality of breakthrough SARS-CoV-2 infection in vaccinees should be taken into full account. Some of the concepts and practices implemented by different countries and economies have their own merits and should not be blindly criticized. For example, Israel and Singapore are taking the lead internationally in the vaccination campaign and in the execution of the “living with SARS-CoV-2” policy. Their hard-learned lessons should be treasured by others. Even if the same policies will not be adopted today, other countries and economies might encounter the same dilemmas and challenges in future.
Above we have revisited the top nine important questions and related issues about SARS-CoV-2 and COVID-19. This pandemic has lasted two years and costed millions of lives. In our opinion, the beginning of the end of the pandemic is already in sight. As in the history, pandemics caused by the other four coronaviruses would be over when the virus became highly adapted in humans and when herd immunity developed in human populations was sufficiently strong. Whereas evidence-based mitigation measures have reduced the damage caused by the pandemic, research efforts have already made a difference in multiple fronts of our battle against SARS-CoV-2 and COVID-19. Importantly, the vaccination schemes have already accelerated the end of the pandemic. Development of next-generation vaccines and innovative use of existing vaccines in combination might ultimately lead to eradication of SARS-CoV-2. We therefore remain guardedly optimistic.
Acknowledgements
We thank Pearl Chan, Terence Lee, Chon Phin Ong and Kam-Leung Siu for critical reading of the manuscript.
Author contributions
KSY and DYJ wrote the manuscript with inputs from ZWY, SYF, PHHC and CPC. All authors read and approved the final manuscript.
Coronavirus research in our laboratory was funded by grants from the Hong Kong Health and Medical Research Fund (COVID190114) and Hong Kong Research Grants Council (C7142-20GF and T11-709/21-N).

Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate, consent for publication, competing interests.
No potential conflict of interest was reported by the authors.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- 1. Yuen KS, Ye ZW, Fung SY, Chan CP, Jin DY. SARS-CoV-2 and COVID-19: The most important research questions. Cell Biosci. 2020;10:40. doi: 10.1186/s13578-020-00404-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. He Z, Ren L, Yang J, Guo L, Feng L, Ma C, et al. Seroprevalence and humoral immune durability of anti-SARS-CoV-2 antibodies in Wuhan, China: a longitudinal, population-level, cross-sectional study. Lancet. 2021;397:1075–84. doi: 10.1016/S0140-6736(21)00238-5. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Chan JFW, Yuan S, Kok KH, To KKW, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–23. doi: 10.1016/S0140-6736(20)30154-9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Sun K, Wang W, Gao L, Wang Y, Luo K, Ren L, et al. Transmission heterogeneities, kinetics, and controllability of SARS-CoV-2. Science. 2021;371(6526):eabe2424. doi: 10.1126/science.abe2424. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Scobie HM, Johnson AG, Suthar AB, Severson R, Alden NB, Balter S, et al. Monitoring incidence of COVID-19 cases, hospitalizations, and deaths, by vaccination status—13 U.S. jurisdictions, April 4–July 17, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1284–1290. doi: 10.15585/mmwr.mm7037e1. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Clark SA, Clark LE, Pan J, Coscia A, McKay LGA, Shankar S, et al. SARS-CoV-2 evolution in an immunocompromised host reveals shared neutralization escape mechanisms. Cell. 2021;184(10):2605-2617.e18. doi: 10.1016/j.cell.2021.03.027. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Kabinger F, Stiller C, Schmitzová J, Dienemann C, Kokic G, Hillen HS, et al. Mechanism of molnupiravir-induced SARS-CoV-2 mutagenesis. Nat Struct Mol Biol. 2021;28:740–746. doi: 10.1038/s41594-021-00651-0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Agostini ML, Pruijssers AJ, Chappell JD, Gribble J, Lu X, Andres EL, et al. Small-molecule antiviral β-d-N4-hydroxycytidine inhibits a proofreading-intact coronavirus with a high genetic barrier to resistance. J Virol. 2019;93(24):e01348-19. doi: 10.1128/JVI.01348-19. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat Med. 2021;27:1205–1211. doi: 10.1038/s41591-021-01377-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Worobey M. Dissecting the early COVID-19 cases in Wuhan. Science. 2021 doi: 10.1126/science.abm4454. [ DOI ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
- View on publisher site
- PDF (833.2 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Visit the Gateway
- Visit the Alliance
- Visit HDR UK Futures
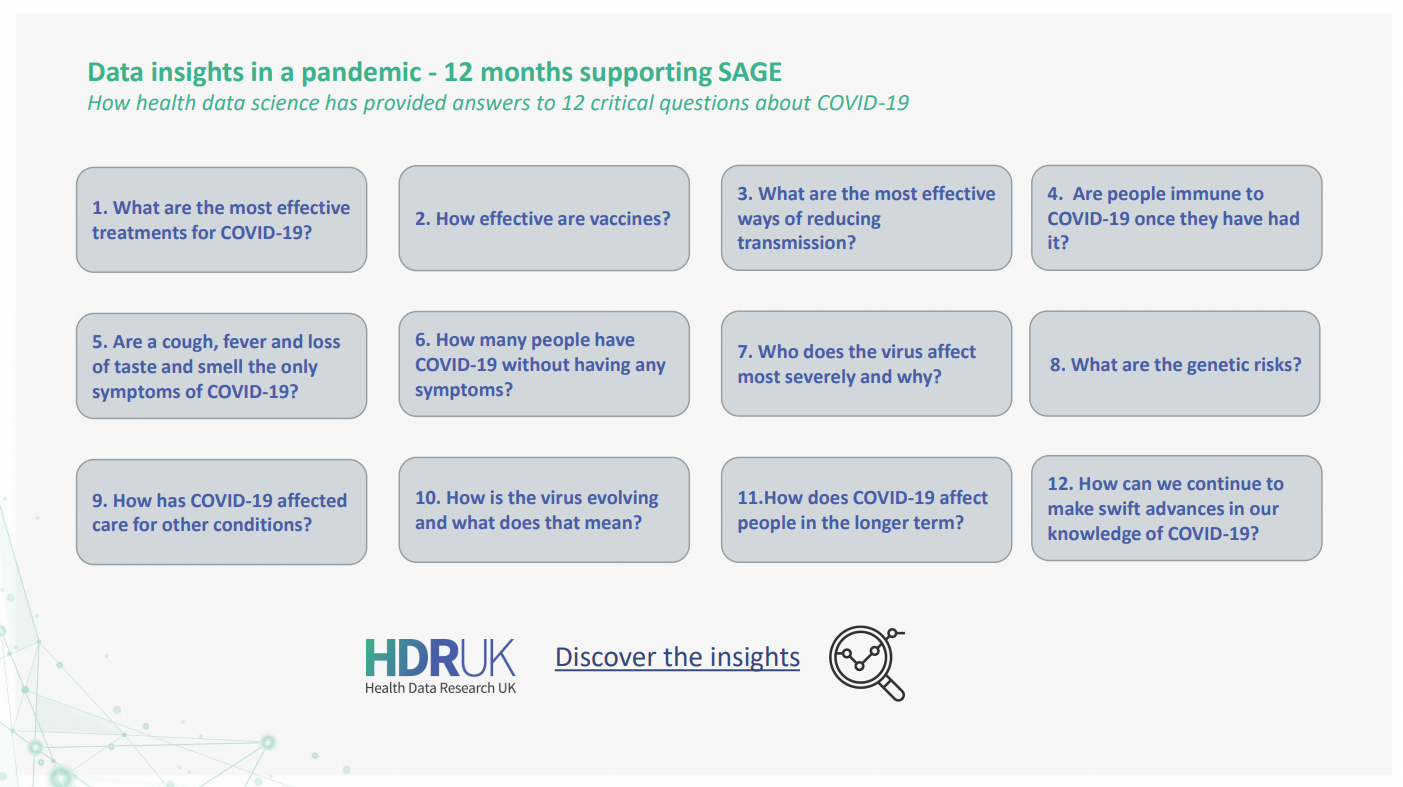
12 crucial questions about COVID-19 answered by health data research
22 April 2021
Data Insights in a Pandemic - 12 months of supporting SAGE
Share this page
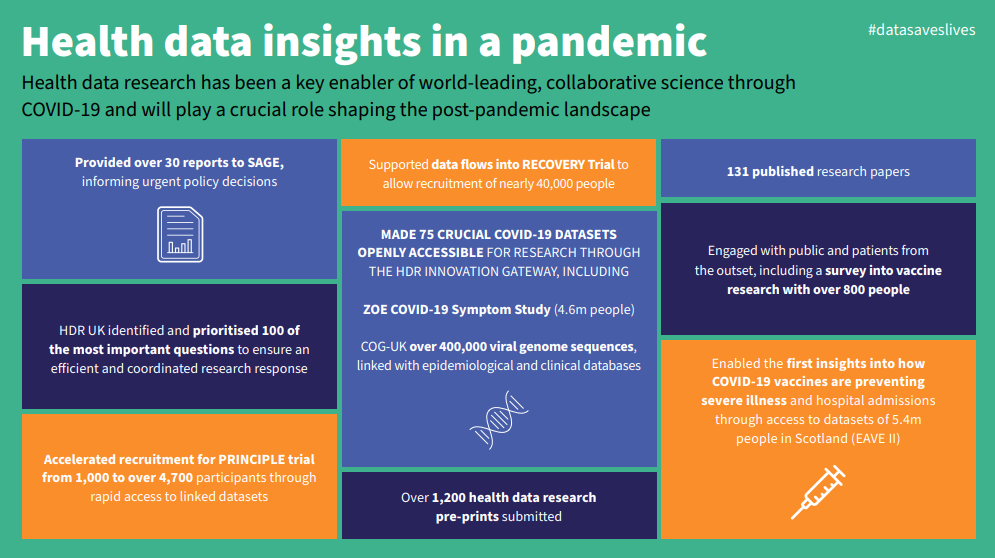
Expert analysis of health data has been central to tackling COVID-19 – showing us how we can reduce its spread, vaccinate against it, and how to most effectively treat people who fall seriously ill.
As the UK gradually emerges from lockdown, 12 months on from the first, there is now greater recognition of the contribution that health data science has made to the progress in tackling COVID-19. When cases first emerged in the UK, very little was known about this virus. Today we have evidence on who is most seriously impacted by COVID-19; how we can most effectively stop its spread, including through vaccines; and which drugs are most effective when people do become seriously ill with the virus.
Some of these breakthroughs have made unlikely household names of clinical trials and many epidemiologists. Perhaps less well-known is the work of the UK’s dedicated health data research community, which has enabled many of these discoveries to take place. By ensuring key datasets are made safely available, analysing those large quantities of data and converting that analysis into actionable insights, their work has formed the backbone of the UK’s ability to tackle the pandemic and keep people well.
The UK collects large quantities of health data. Used safely, it is a valuable asset. But the datasets are fragmented, residing in multiple locations, meaning it can be hard and time consuming for scientists to find and access.
Health Data Research UK (HDR UK) – the country’s national institute for health data science – addresses these challenges, by uniting data and helping coordinate research efforts. In the past 12 months, it has made sure researchers can quickly access information relevant to COVID-19. This has enabled experts to make swift breakthroughs.
HDR UK has also ensured these findings are rapidly shared with national decision makers. The government’s Scientific Advisory Group on Emergencies (SAGE) has received 28 reports from HDR UK and its partners since April 2020. These reports detail the new datasets being made available and summarise key COVID-19 research. This means those influencing or making national policy have the information they need to make the best possible decisions.
“Data saves lives, as the pandemic h as starkly illustrated. By continuing to bring the health research community together to use data in a trustworthy way– and engaging with members of the public – HDR UK will help shape the post-pandemic research landscape and support the future development of health data science, both in the UK and globally.” Caroline Cake, Chief Executive , Health Data Research UK
To find out more about how health data science has been central to tackling COVID-19, sign up for HDR UK’s annual Scientific Conference Data Insights in a Pandemic on 23 June and our National Core Studies Symposium on 24 June .
Twelve important questions health data research has helped answer:
1. what are the most effective treatments for severe covid-19.
For h ospitalised patients:
Dexamethasone – arguably the research breakthrough of the last 12 months from RECOVERY as a unique, data-enabled trial that came together at breakneck speed , using data via NHS DigiTrials , based on:
- Rapidly expediated data governance
- Expertise provided by HDR UK’s data-enabled Clinical Trials work developed over the previous two years
- W e also know that tocilizumab reduces the risk of death in patients who are hospitalised with severe COVID-19 ; and that sarilumab does the same . These studies informed updated guidance recommending the use of tocilizumab for any patient admitted to intensive care with COVID-19.
Non-hospitalised patients: Another HDR UK supported, data-enabled trial – PRINCIPLE – has provided the insight that asthma drug budesonide shortens recovery time in non-hospitalised patients .
2. How effective are vaccines against COVID-19?
Thanks to health data research ers working at pace , including those supported by HDR UK, we were able to know as quickly as 22 February that the vaccines scientists have developed against COVID-19 are effective:
- A single dose of the Oxford/AstraZeneca vaccine is 94% effective against COVID-19 related hospitalisation
- A single dose of the Pfizer/BioNTech vaccine is 85% effective against COVID-19 related hospitalisation
- The Pfizer/BioNTech vaccine reduces infection rates by 75% after a single dose
- Older people who have been vaccinated are 50% less likely to be hospitalised or die due to COVID-19
We also know that vaccination rates are lower in people from an ethnic minority background, who liv e in areas of higher deprivation, and who have severe mental illness or learning disabilities . This helps healthcare leaders understand where they will need to make special efforts to encourage vaccine uptake.
Thankfully, we also know that this can change. Data from over 20,000 adults as part of the VirusWatch household study indicate that 86% of participants who were reluctant or intending to refuse a COVID-19 vaccine in December were planning on accepting (or already had accepted) a vaccine in February – and these findings were consistent across ethnic and social groups. This shift in attitude highlights the need to offer vaccines repeatedly as people change their minds over time .
3. What are the most effective ways of reducing transmission of COVID-19?
Asking people to work from home was found to have been the most effective method of reducing social contact in summer and autumn 2020 .
So long as strict mitigation measures were in place, teachers in Wales and in England were shown to have been at no increased risk of COVID-19 infection as schools reopened.
4. Are people immune to COVID-19 once they have had it?
It seems antibodies from COVID-19 provide some immunity to reinfection, lasting for at least five months. But antibody levels have been shown to decrease fairly quickly, particularly in younger adults and those who had no symptoms .
5. Are a cough, fever and loss of taste and smell the only symptoms of COVID-19?
Research has shown chills, loss of appetite, headache and muscle ache are also strongly linked with COVID-19 infection.
6. How many people have COVID-19 without having any symptoms?
19% of people who test positive for COVID have no symptoms at all, and 27% do not have the core symptoms of fever, cough or loss of taste and smell .
20% of people will have no symptoms at any point in their infection, but most people with COVID-19 will have some symptoms at some point .
This shows that even people who feel well may have the virus and be at risk of spreading it to others.
7. Who does the virus affect most severely and why?
Research has shown us that certain groups are much more likely to be badly affected by the virus. This includes:
- People with intellectual disabilities
- People who are older, male, overweight or from a deprived background
- People who have migrated to high income countries
- Orthodox Jewish populations (a study suggested an infection rate of five times the estimated national rate)
We also know that people from black and minority ethnic backgrounds are at higher risk , though the level of risk has changed as the pandemic has progressed .
And health data research has revealed some of the reasons these groups might be more at risk from COVID-19. The use of new large datasets, in this case the ZOE Covid Symptom Study ( validated by further key datasets such as ONS Community Infection Survey), have been able to shed light on the geographic incidence of the virus , helping to detect rapid case increases in regions where government testing provision was lower. Such data provides an agile resource, part of a basket of indicators being used by policy makers during a quickly moving pandemic.
See latest research here
8. What are the genetic risks?
We know about genetic risks too. And n ot just increased ris k – d ata from over 2000 participants of the Genetics Of Mortality In Critical Care (GenOMICC) and the International Severe Acute Respiratory Infection Consortium (ISARIC) Coronavirus Clinical Characterisation Consortium (4C) (ISARIC 4C) studies indicate that a common variant of the protein occurring in approximately 25% of the population is associated with a reduced likelihood of developing severe COVID-19 – suggesting that this protein ( TMPRSS2 ) is a promising drug target in the treatment of COVID-19.
9. How has COVID-19 affected care for other conditions?
Using large-scale datasets from HDR UK hubs including Data-CAN and the BHF Data Science Centre , h ealth data research has shown that:
- There were fewer interactions with GPs during the first part of the pandemic
- There have been decreases in heart disease referrals, diagnoses and treatment
- There have been reductions in referrals for suspected cancer – including colorectal cancer
- There have been decreases in the number of people attending chemotherapy appointments and impact on radiotherapy treatment too
- There is a growing backlog of endoscopic procedures such as colonoscopies that could take more than a year to clear
All of this is important in helping healthcare leaders plan services and care for those living with other serious illnesses during the pandemic.
10. How is the virus evolving and what does that mean?
The UK has carried out nearly half of all the world’s genome sequencing of COVID-19 – which is crucial part of our intelligence about the virus. The UK’s genuine global leadership in genomics is largely thanks to the incredible work of the COVID-19 Genomics UK Consortium “ COG-UK ”, led by Professor Sharon Peacock with the support of HDR UK project management and research expertise in understanding the cause of diseases . Their impact includes , among many other discoveries, the identification of new strains of COVID-19, including the B.1.1.7 (“British” or “Kent” ) variant.
Research from Imperial College London and the CMMID COVID-19 Working Group showed the B.1.1.7 (“British” or “Kent” ) variant is 50% more transmissible, which is important in understanding the current and future danger presented by the virus.
11.How does COVID-19 affect people in the longer term?
- We know there is an increased risk of mortality even following a hospital stay for COVID-19 and a need for further research into the long-term impact of the virus.
- A social media survey of 2550 people , co-produced with people living with long COVID, found that long Covid affected respondents daily life including their mental health, work, and domestic chores. For the majority, symptoms such as exhaustion, breathlessness, headache, and chest pressure/tightness fluctuate or relapse and common triggers include physical activity, stress, sleep disturbance and cognitive activity.
- Patient reported outcomes from 1,000 people discharged from hospital following treatment for COVID-19, revealed most survivors are not fully recovered five months after discharge – around 1 in 5 people developed a new disability, stopped working or changed jobs due to their health, and/or experienced symptoms of anxiety or depression .
12. How can we continue to make swift advances in our knowledge of COVID-19?
Researchers have used data to more rapidly recruit people to clinical trials . The accelerated recruitment to trials such as RECOVERY and PRINCIPLE has been one of the undoubted success stories to have emerged from a global health crisis; and will surely be one of the enduring aspects that will continue to be of benefit for years to come.
For now, continuing to use these techniques – the application of large-scale datasets to support recruitment and maintain participation in these trials – will be key to advance our understanding of how best to prevent and treat COVID-19.
Our Work to Help SAGE
We work with the Strategic Advisory Group for Emergencies (SAGE) by providing SAGE with prioritised health data research related to COVID-19.
COVID-19 Data and Connectivity
Data and Connectivity connects UK health data, accelerating research on COVID-19 and enabling stronger, research evidence-informed policies for COVID-19 response, pandemic recovery and future...

False Positive Tests
"False positives" have been an issue since testing for COVID-19 pandemic began. As the volume of tests has significantly increased, it has become even more relevant. Find out more in this piece by...
Our funders

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 15 February 2023
Coronavirus research: knowledge gaps and research priorities
- Stanley Perlman ORCID: orcid.org/0000-0003-4213-2354 1 &
- Malik Peiris ORCID: orcid.org/0000-0001-8217-5995 2 , 3
Nature Reviews Microbiology volume 21 , pages 125–126 ( 2023 ) Cite this article
6832 Accesses
7 Citations
16 Altmetric
Metrics details
- Policy and public health in microbiology
Decades of coronavirus research and intense studies of SARS-CoV-2 since the beginning of the COVID-19 pandemic have led to an unprecedented level of knowledge of coronavirus biology and pathogenesis, yet many outstanding questions remain. Here, we discuss knowledge gaps and research priorities in the field.
Introduction
The COVID-19 pandemic showed that, based on previous research efforts, we understood many aspects of coronavirus biology and pathogenesis, but also that there was much we did not know. In 2019, the worldwide number of coronavirus investigators was small, having increased after the severe acute respiratory syndrome coronavirus (SARS-CoV) outbreak in 2003 but decreasing thereafter. The influx of scientists with diverse expertise into the field after the pandemic onset contributed to an increased understanding of coronavirus replication, epidemiology, SARS-CoV-2 pathogenesis and immune responses in humans, to the development and characterization of experimentally infected animal models for COVID-19, and to SARS-CoV-2 vaccine and antiviral drug development. Here, as investigators who have studied coronaviruses for decades, we outline some of the outstanding research questions that we think need to be addressed.
SARS-CoV-2 emergence
Where did SARS-CoV-2 originate and how did it evolve to infect humans? The emergence of SARS-CoV-2 continues to be an area of controversy and has been, and is being, investigated by many national and international organizations, including the WHO (World Health Organization). It is almost certain that the virus originated in bats and crossed species to humans either directly or indirectly via intermediary hosts. There remains debate on whether the virus first infected humans from a zoonotic source or from a research laboratory, but, no matter what the answer to this question is, it is clear to us that in order to be prepared for the next pandemic, we need to further delineate the panoply of coronaviruses present in bats and possible intermediary hosts 1 . We need to better understand coronavirus circulation in hotspots, such as parts of China and Southeast Asia, where humans, wildlife gathered for food or medicinal purposes and bats are in close proximity. These investigations should include surveillance (virological and serological) of humans in close contact with bats and the game animal trade, with or without respiratory disease, for evidence of coronavirus infection. A related question, discussed below, is why coronaviruses are especially good at jumping species, to humans and other animals.
Zoonotic risk
Once coronaviruses in animal reservoirs are identified, can they be better risk assessed for threats for human spillover? Surveillance of bat reservoirs of sarbecoviruses (Sarbecovirus is the subgenus to which SARS-CoV-2 belongs) had previously found evidence of viruses with a capacity for infecting human cells using the angiotensin converting enzyme 2 (ACE2) receptor (reminiscent of SARS-CoV) 2 . Serological evidence of viral spillover to humans was demonstrated before the emergence of SARS-CoV-2 (ref. 3 ). Arguably, these signals together should have been triggers for action to develop countermeasures with greater urgency. The availability of human organoid cultures and ex vivo cultures of human respiratory tissue may enable the use of physiologically relevant systems for a more systematic risk assessment of animal coronaviruses in the future, analogous to ongoing risk assessments being carried out for animal influenza viruses 4 .
SARS-CoV-2 transmissibility
What explains the high transmissibility of SARS-CoV-2 compared with SARS-CoV or Middle East respiratory syndrome coronavirus (MERS-CoV)? A critical factor leading to the COVID-19 pandemic was the ability of SARS-CoV-2 to grow to high levels in the upper respiratory tract and therefore to readily transmit to other humans. Titres of SARS-CoV and MERS-CoV in the upper respiratory tract peak at later times after infection 5 , consistent with the ability to interrupt transmission with relevant public health infection-prevention methods. A second, related question is why SARS-CoV and a common cold coronavirus, HCoV-NL63, which both use the same receptor as SARS-CoV-2 (ACE2) 6 , have such different patterns of infection within the human respiratory tract. HCoV-NL63 rarely infects the lower respiratory tract, whereas SARS-CoV preferentially causes pneumonia. These different patterns of infection most likely relate to differences in cell entry, including differences in co-receptor usage, host protease usage or fusogenicity of the spike protein, but there are other possibilities. Understanding these differences will provide information on which coronavirus might be expected to be transmissible and to identify additional targets for therapeutic interventions. Further elucidation of the factors that contribute to virus spread will require additional experimental animal models of coronavirus transmission.
The SARS-CoV-2 outbreak also highlighted the lack of evidence-based data on the transmission of coronaviruses, or indeed respiratory viruses in in general, and on which non-pharmaceutical countermeasures (for example, social distancing and masks (surgical versus N99/FFP3 masks)) are effective or not. The SARS-CoV-2 outbreak demonstrated that the only effective control options available in the first months of the pandemic were non-pharmaceutical, but our understanding of the efficacy of specific measures is limited.
Coronavirus genome complexity
Why do coronavirus genomes encode so many more proteins than other RNA viruses? Coronavirus genomes are bigger than those of any other RNA virus, apart from those of related members of the Nidovirales order. The genomes are so large that they require genomic proofreading activity to avoid error catastrophe 7 . A large genome size may contribute to enhanced cross-species transmission, but, at present, this notion is speculative. In any case, an important question is to understand the function of the many non-structural proteins involved in virus replication. Development of a cell-free or entirely in vitro replication system would facilitate detailed probing of the role of individual proteins in replication and transmission. Efforts to develop such cell-free systems were initiated 40 years ago, but it is only in the past few years with the advent of cryo-electron microscopy and new biochemical approaches that progress has been made. These efforts are expected to complement studies in intact cells, which use high-resolution microscopy and related techniques to analyse macromolecular interactions and function at the subcellular level.
Related to the previous question, why do coronaviruses encode so many proteins with apparent immunoevasive function? Coronaviruses encode a variable number of accessory proteins, the genes of which are intermingled within the structural protein genes located at the 3′ end of the genome. For example, SARS-CoV-2 encodes at least six such proteins, with several other putative open reading frames in the genome hypothesized to be expressed and have immunoevasive properties 8 . Confusingly, these genes are often deleted in viruses isolated from infected animals, without apparent loss of virulence. This was shown most clearly in the case of MERS-CoV, in which diverse deletions and insertions in accessory genes were detected in some isolates obtained in Africa from camels, the primary host of the virus 9 . These genetic changes may have unpredictable consequences for virus transmissibility or pathogenesis. Deletion of these genes occasionally leads to increased virulence 10 . The variable and sometimes unexpectedly high numbers of these proteins suggest that they have redundant and, perhaps, additional functions. Such redundancy could contribute to cross-species transmission. The genetic instability of MERS-CoV camels in Africa therefore needs to be monitored and evidence for human spillover needs to be continually assessed.
Predictive evolution
Can coronavirus evolution in infected human or other animal hosts be predicted? Coronaviruses readily mutate and recombine as they adapt to a new host. This is well illustrated by the COVID-19 pandemic, in which ancestral strains of SARS-CoV-2 initially mutated to better infect humans, and later evolved to evade the human immune response, generating a series of variants of concern. Several studies have modelled SARS-CoV-2 evolution but so far it has not been possible to predict how the virus will evolve in the future. Such predictive modelling is recognized to be difficult, but would be very useful in the present pandemic as well as in future coronavirus outbreaks or pandemics for vaccine development, for anticipating clinical disease and pathogenesis, and for risk assessment of animal viruses with zoonotic potential.
Keusch, G. T. et al. Pandemic origins and a One Health approach to preparedness and prevention: solutions based on SARS-CoV-2 and other RNA viruses. Proc. Natl Acad. Sci. USA 119 , e2202871119 (2022).
Article CAS PubMed PubMed Central Google Scholar
Menachery, V. D. et al. A SARS-like cluster of circulating bat coronaviruses shows potential for human emergence. Nat. Med. 21 , 1508–1513 (2015).
Li, H. et al. Human-animal interactions and bat coronavirus spillover potential among rural residents in Southern China. Biosaf. Health 1 , 84–90 (2019).
Article PubMed PubMed Central Google Scholar
Cox, N. J., Trock, S. C. & Burke, S. A. Pandemic preparedness and the Influenza Risk Assessment Tool (IRAT). Curr. Top. Microbiol. Immunol. 385 , 119–136 (2014).
PubMed Google Scholar
Cevik, M. et al. SARS-CoV-2, SARS-CoV, and MERS-CoV viral load dynamics, duration of viral shedding, and infectiousness: a systematic review and meta-analysis. Lancet Microbe 2 , e13–e22 (2021).
Article CAS PubMed Google Scholar
Hofmann, H. et al. Human coronavirus NL63 employs the severe acute respiratory syndrome coronavirus receptor for cellular entry. Proc. Natl Acad. Sci. USA 102 , 7988–7993 (2005).
Eckerle, L. D., Lu, X., Sperry, S. M., Choi, L. & Denison, M. R. High fidelity of murine hepatitis virus replication is decreased in nsp14 exoribonuclease mutants. J. Virol. 81 , 12135–12144 (2007).
Lowery, S. A., Sariol, A. & Perlman, S. Innate immune and inflammatory responses to SARS-CoV-2: implications for COVID-19. Cell Host Microbe 29 , 1052–1062 (2021).
Chu, D. K. W. et al. MERS coronaviruses from camels in Africa exhibit region-dependent genetic diversity. Proc. Natl Acad. Sci. USA 115 , 3144–3149 (2018).
Gutierrez-Alvarez, J. et al. Middle East respiratory syndrome coronavirus gene 5 modulates pathogenesis in mice. J. Virol. 95 , e01172-20 (2021).
Download references
Author information
Authors and affiliations.
Department of Microbiology and Immunology, University of Iowa, Iowa City, IA, USA
Stanley Perlman
HKU-Pasteur Research Pole, The University of Hong Kong (HKU), Hong Kong Special Administrative Region, People’s Republic of China
Malik Peiris
School of Public Health, Li Ka Shing Faculty of Medicine, The University of Hong Kong (HKU), Hong Kong Special Administrative Region, People’s Republic of China
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Stanley Perlman .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Perlman, S., Peiris, M. Coronavirus research: knowledge gaps and research priorities. Nat Rev Microbiol 21 , 125–126 (2023). https://doi.org/10.1038/s41579-022-00837-3
Download citation
Published : 15 February 2023
Issue Date : March 2023
DOI : https://doi.org/10.1038/s41579-022-00837-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Dynamic label-free analysis of sars-cov-2 infection reveals virus-induced subcellular remodeling.
- Nell Saunders
- Blandine Monel
- Mathieu Fréchin
Nature Communications (2024)
SARS-CoV-2 and innate immunity: the good, the bad, and the “goldilocks”
- Benjamin L. Sievers
- Mark T. K. Cheng
- Ravindra K. Gupta
Cellular & Molecular Immunology (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Microbiology newsletter — what matters in microbiology research, free to your inbox weekly.
Key ethical questions for research during the COVID-19 pandemic
Affiliations.
- 1 Self-Harm Research Group, School of Psychology, University of Nottingham, Nottingham NG7 2RD, UK. Electronic address: [email protected].
- 2 Self-Harm Research Group, School of Psychology, University of Nottingham, Nottingham NG7 2RD, UK.
- 3 College of Medicine and Veterinary Medicine, University of Edinburgh, Edinburgh, UK.
- 4 Self-Harm Research Group, School of Psychology, University of Nottingham, Nottingham NG7 2RD, UK; Mental Health in Autism Research Group, School of Psychology, University of Nottingham, Nottingham NG7 2RD, UK.
- PMID: 32353264
- PMCID: PMC7185919
- DOI: 10.1016/S2215-0366(20)30150-4
- Betacoronavirus
- Biomedical Research / trends
- Coronavirus Infections* / epidemiology
- Coronavirus Infections* / psychology
- Ethics, Research*
- Mental Health*
- Pneumonia, Viral* / epidemiology
- Pneumonia, Viral* / psychology

IMAGES
COMMENTS
COVID-19 CLINICAL TRIAL RECOMMENDATIONS-As multiple federal research agencies have demonstrated, it is most ethical and prudent to enroll patients with COVID-19 in clinical trials rather than use clinically unproven therapies. There are multiple ongoing trials, some with adaptive designs, which potentially can quickly answer pressing questions on
8 Major Findings and Research Questions INTRODUCTION. The COVID-19 pandemic, which began in late 2019, created unprecedented global disruption and infused a significant level of uncertainty into the lives of individuals, both personally and professionally, around the world throughout 2020.
This applies to COVID-19 as well. In fact, this understanding could save your life. When President Trump touted the advantages of hydroxychloroquine as a way to prevent and treat COVID-19, he was dramatically overstating the results of one observational study. Later studies with control groups showed that it did not work—and, in fact, it didn ...
The sixth question concerns how COVID-19 should be treated and what treatment options should be made available. COVID-19 is a self-limiting disease in more than 80% of patients. Severe pneumonia occurred in about 15% of cases as revealed in studies with large cohorts of patients. The gross case fatality is 3.4% worldwide as of February 25, 2020.
When only slightly more than 80,000 confirmed cases of SARS-CoV-2 infection were reported worldwide and right before COVID-19 was declared a pandemic by the WHO, we discussed the nine most important research questions on SARS-CoV-2 and COVID-19, in our commentary that was published in Cell & Bioscience at the end of February 2020 [].These questions are:
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an ongoing global health emergency. Here we highlight nine most important research questions concerning virus transmission, asymptomatic and presymptomatic virus shedding, diagnosis, treatment, vaccine development, origin of virus and ...
Twelve important questions health data research has helped answer: 1. What are the most effective treatments for severe COVID-19? For h ospitalised patients: . Dexamethasone - arguably the research breakthrough of the last 12 months from RECOVERY as a unique, data-enabled trial that came together at breakneck speed, using data via NHS DigiTrials, based on:
One unexpected challenge early in the pandemic was the stigma associated with COVID-19. Some people were reluctant to get tested, fearing isolation or quarantine.
The COVID-19 pandemic showed that, based on previous research efforts, we understood many aspects of coronavirus biology and pathogenesis, but also that there was much we did not know.
Key ethical questions for research during the COVID-19 pandemic. Key ethical questions for research during the COVID-19 pandemic. Key ethical questions for research during the COVID-19 pandemic Lancet Psychiatry. 2020 May;7(5):381-383. doi: 10.1016/S2215-0366(20)30150-4. ...